Claims Cheat Sheet
General Claims Information
- Claims are processed according to the State HFS (Medicaid) or CMS (Medicare) fee schedule
- Claims can be submitted via Web Portal, Clearinghouse, or RED Paper Claim form.
- UB-04 claim form is used to file Hospital (inpatient and outpatient) LTC and SNF claims
- CMS 1500 claim form is used to file office visits, outpatient and ancillary claims
- National Drug Code (NDC) – The number submitted on a claim that is billed with J and Q codes
Required Data Elements
| Element | Element Information |
|---|---|
| National Drug Code (NDC) | NDC format (5-4-2) |
| Drug Unit of Measure (UOM) | Valid unit of measures are: F2 (international unit) / GR (gram) / ML (milliliter) / UN (unit) / ME (Milligram) |
| Drug unit quantity | Dispensing quantity |
- National Provider Identifier (NPI) - This number is required for all medical professionals and not required for A-Typical providers (HCBS non-medical professionals-ie Homemaker, Adult Day Care, Supportive Living)
- Patient Credit File (PCF) – If a claim is denied due to patient not on credit file “DO NOT” have the provider resubmit the claim. Payment will be released once the member is added to the file by the State.
- Present on Admission (POA) – Providers must include the POA indicator for each diagnosis billed for Inpatient claims. If the POA indicator is missing or invalid the entire claim will be denied. If there is a diagnosis which was not present on admission, a $900 penalty will be assessed. POA indicators are not required for LTC/SNF providers.
Service Package 1 (SPI)
- Use claim form CMS 1500.
- Authorizations may not be required for some DME purchases greater than $500 as long as it’s a covered benefit; verify the cpt/hcpc code on ILYouthCare.com. $500 is based on the HFS fee schedule amount per claim line.
- Authorizations are required regardless of cost for oxygen, bi-pap, c-pap, 02 concentrator, ventilator, wound vac, bone growth stimulators, neuro stimulators, custom wheelchairs and scooters.
- Provider must not exceed the allowed amounts. If the equipment is hand priced (no published rate) YouthCare will only reimburse a percentage % of billed charges.
- Inpatient claims are submitted on a UB-04.
- Payments include two methods of reimbursement: per diem and DRG.
- Under DRG, YouthCare reimburses the hospital based on the diagnoses and procedures performed during the hospital stay. The diagnoses associated with the hospital stay are placed into groups requiring a similar intensity of services.
- Under per diem methodology, hospitals receive a flat rate for each day of inpatient services provided.
- Reimbursement is based on the date of admission. If patient coverage terms during the inpatient stay, the plan YouthCare at time of admission is responsible for the entire inpatient stay. There are a few exceptions: Skilled Nursing/LTC, professional fees (office visits, outpatient) are paid according to effective date of coverage.
- Providers must submit Outpatient APL codes on a UB-04. ALL other non-APL codes must be submitted on a 1500 claim form.
- The type of bill will determine the type of claim.
- Outpatient payments are made to hospitals using the procedure grouping: The department refers to this program as the Ambulatory Procedures Listing (APL).
- A listing of procedures that has been determined by the department of HFS to be either unique to or most appropriately provided in the hospital outpatient or ambulatory surgical treatment center setting.
- Reimbursement is based on a case rate by procedure code. The list of appropriate APL codes can be found on the HFS website.
- One APL is payable per date of service. For example, if a member enters the hospital via the emergency room on 10/15 but is transferred to an observation bed on 10/16, the APL rate is paid both for the ER and observation APL codes.
- Claims are submitted on a HCFA 1500.
- All services are billed with HCPCS code T1015 on the first claim line.
- Services are reimbursed at the all inclusive encounter rate assigned by HFS to the group.
- Use claim form UB-04.
- Hospice provider must bill admit date, value codes and CBSA codes on their claims.
- Room and board for members receiving hospice services in a long term care facility are handled as pass-through billing by the hospice provider.
- A Notification of Election form must be submitted to YouthCare and the State of Illinois and must be on file before claims are reimbursed.
- Claims cannot be released for payment if the member and hospice provider are not listed on the Patient Credit File.
- If the member is residing in a LTC facility, YouthCare will pay the LTC facility’s per diem rate to the hospice agency and the hospice agency is responsible for paying the LTC facility. This arrangement must be agreed upon between the hospice agency and the LTC facility. YouthCare is not part of this negotiation.
- MTM - Non-Emergent Non-Ambulance Transportation.
- Needs verification by MTM.
- Emergency transportation services are ONLY billable to YouthCare.
- Non-emergency transportation providers must have a contract on file with MTM and submit claims directly to MTM's claims office.
- Use claim form CMS 1500.
- Authorizations are required for all services
- Providers can submit claims for RN visits, PT, OT and ST
- Home Health SPI services are billed in units per visit; example 1 day = 1 unit.
- Providers will use the member’s medical diagnosis (DX) for SPI services.
Service Package 1 (SPII) - Waiver Services
- Use claim form CMS 1500.
- Medicaid benefit only.
- Services are billable for members that qualify for waiver services.
- The initial assessment, eligibility and the Determination of Need (DON) score is determined by the Dept. of Rehabilitations (DRS) or Dept. On Aging (DOA).
- A combination of the DON score and waiver program determines the services a member may receive and the allotted hours/days/dollars.
- Members have a choice to accept or decline services and the right to choose a provider.
- Continuity of care applies, therefore waiver services and the associated providers will remain in place 180 days.
- Personal Assistants are still the responsibility of the State and not billable to YouthCare.
- All providers will use a non-medical diagnosis code of Dx:V68.81 for waiver services.
- Use claim form CMS 1500.
- Medicaid benefit only.
- YouthCare covers the waiver services included in the Supportive Living Facility (laundry, personal care, maintenance, etc.) at a per diem rate but does not pay for room and board.
- Providers will bill using a non-medical diagnosis code of Dx:V68.81 and Procedure code T2033 for all members.
- Leave of absence days (whether to go to the hospital or therapeutic) are payable at 100% of the assigned rate for 30 days per calendar year. LOA should be billed with T2033-U1.
- Use claim form CMS 1500.
- Authorizations are required for all services.
- Providers can submit claims for RN visits, PT, OT and ST.
- Home Health SPII services covered under the waiver program must refer to the HCBS increment grid. Units are billed per 15min. increments; example 1 hour = 4 units.
- Providers will use DX: Z04.9 for all SPII waiver services unless a medical diagnosis is given.
Long Term Care (LTC) & Skilled Nursing Facility (SNF)
- Use claims form UB-04.
- Authorizations are required for ALL services.
- Custodial Care is a Medicaid covered benefit ONLY.
- Custodial members reside at the LTC or SNF facility and is intended to stay long-term.
- Skilled Care is subject to service limitations. If patient becomes Custodial during the members stay the LTC/SNF must complete and submit an 1156 form to the State of Illinois as notification of a custodial admission. The provider will also need to notify YouthCare and obtain another authorization.
- Skilled Care and Custodial Care is reimbursed at the same per diem rate for ICP/FHP members.
ICP and FHP: Therapy services are covered in the per diem rate. Services are covered ONLY if rendered and billed by an entity other than the long term care facility and are deemed medically necessary.
MMP / MMAI / Duals: If the member is an MMP member and the therapy is considered a Part B service, then therapy claims should be billed to YouthCare.
- Services must be pre-authorized and are subject to service limitations.
- If this is not a Part B service or if Part B has been exhausted, LTC facilities will not be reimbursed for therapy. Services are covered ONLY if rendered and billed by an entity other than the long term care facility and are deemed medically necessary.
- Use claim form CMS 1500.
- LTC facilities are responsible for providing the 1st tank of oxygen on a monthly basis and are not allowed to bill for the 1st tank.
- LTC facilities must be registered as a DME provider type 63 with the State.
- If you are not registered as a provider type 63 for DME, claims will deny.
- Oxygen claims must be billed separately from the Room & Board claim and submitted on a 1500 professional claim form.
- YouthCare can only pay claims for members and days on the State’s PCF.
- All custodial care claims refer to the patient credit file to deduct member funds accordingly.
- Ex code on the Explanation of Payment (EOP): Hf
- Description: “DENY”: Mbr not currently on PT Credit File – will reconsider once on file.”
- Claim does NOT need to be resubmitted.
- Claims will be paid as soon as member appears on patient credit.
- If providers have any questions about a member residing in a facility, they can contact Provider Relations at: 844-289-2264 (TTY: 711).
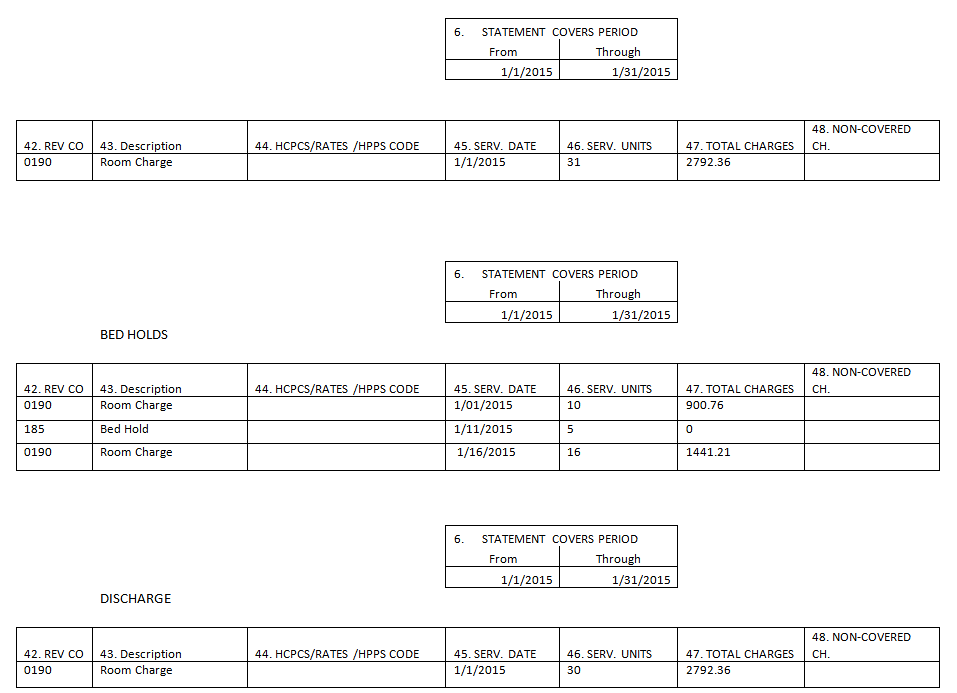
Bed holds are not reimbursable under the 2012 SMART Act but the hold days MUST be billed if included in the overall days.
Sub-Acute Care:
- 0191 sub-acute care – Level I UB04 Revenue Code
- 0192 sub-acute care – Level II UB04 Revenue Code
- 0193 sub-acute care – Level III UB04 Revenue Code
- 0194 sub-acute care – Level IV UB04 Revenue Code
- 0199 other sub-acute care UB04 Revenue Code
- 019X sub-acute care UB04 Revenue Code
Custodial Care:
- 0120 or 0190 general classification UB04 Revenue Code
- Other revenue codes that are appropriate for custodial care
Bed Holds:
- 185 – Nursing Home (for hospitalization)
- 183 – Therapeutic Leave
- 18X other revenue codes that are appropriate for bed holds
Bill Types:
- 212 – 1st claim
- 213 – Interim continuing claim
- 214 – Interim last claim
- 217 – Replacement of prior claim