Resolving Common Claims Rejections
Date: 05/13/25
YouthCare Claims Operations provides guidance on common claims rejection reasons to assist providers in quickly resolving rejected claims. A rejected claim is a claim that has missing or insufficient information that will prevent the claim from entering the claim system.
Learn more from the: Illinois Association of Medicaid Health Plans Comprehensive Billing Manual.
REJECTED CLAIMS GUIDELINES
If a claim is rejected and you are correcting a field and re-submitting the changed claim, submit the claim as a first-time claim. Rejections are not proof of timely submissions. Rejected claims must be resolved and resubmitted within 180 days from the date of service (DOS) timely filing guidelines.
COMMON REJECTIONS
02 REJECTION: Invalid MBR
ISSUE: A member is not valid for the date of service (DOS) being billed.
RESOLUTION:
- Step 1: Review the member's RIN for the date range (month of the claim) in the IL MEDI System
- Step 2: If MEDI shows that the member is enrolled with Meridian or YouthCare, contact Provider Services for assistance. Provider Services will request that the member’s eligibility be updated and a case number will be issued.
- Step 3: Submit a first time claim once the member’s eligibility has been updated, within 180 days from date of service
- Step 4: If MEDI does not show the member enrolled with Meridian or YouthCare, bill the correct plan shown in MEDI
09 REJECTION: Member Invalid on Date of Service
ISSUE: Member is not showing effective for the DOS billed. The member may have coverage through another carrier, or an update was not transmitted to the plan from the state.
RESOLUTION:
- Step 1: Review the member’s RIN in the IL MEDI System for the date range (month of the claim)
- Step 2: If MEDI shows that the member is enrolled with Meridian or YouthCare, contact Provider Services for assistance. Provider Services will request that the member’s eligibility be updated and a case number will be issued.
- Step 3: Submit a first-time claim once member’s eligibility has been updated, within 180 days of date of service
- Step 4: If MEDI does not show the member enrolled with Meridian or YouthCare, bill the correct plan shown in MEDI
01 REJECTION: Invalid Member Date of Birth (DOB)
ISSUE: Member’s date of birth does not match resolution
RESOLUTION:
- Step 1: Verify the DOB submitted on the claim and ensure it matches the DOB in the IL MEDI system
- Step 2: If the DOB is incorrect in MEDI, the member must notify HFS to have their DOB corrected
- Step 3: If DOB was entered incorrectly on the claim, correct the DOB and submit the claim as a first-time claim within 180 days of date of service
- Step 4: Verify the DOB with the plan and MEDI are the same by using a Meridian Provider Portal
- Step 5: If the two systems do not match, contact Meridian or YouthCare Provider Services to have the member information updated with the health plan
- Step 6: After the DOB has been updated, submit a first-time claim within 180 days of date of service
M6 REJECTION Provider Not Valid/Found on State File
ISSUE: Provider billed using a group NPI and/or rendering NPI that is not registered with the state; therefore, the group NPI and/or rendering NPI is not listed on the state provider file
RESOLUTION:
Non-Waiver Providers
- Step 1: Review NPI from claim image against what is in IMPACT to verify the group NPI and rendering NPI are listed and effective for service dates
- Step 2: If NPI is not listed in IMPACT, the provider must enroll in the IMPACT system
- Step 3: If NPI is listed in IMPACT, contact Provider Relations for help with loading the NPI to the Meridian or YouthCare provider system
Waiver Providers
- Step 1: Compare Medicaid number billed in Box 33b from claim image against what is in IMPACT to verify that the Medicaid number is listed and effective for service dates as a waiver provider
- Step 2: If Medicaid number is not listed in IMPACT, the provider must enroll in the IMPACT system
- Step 3: If the Medicaid number is listed in IMPACT, contact Provider Relations for help to get the NPI loaded to the Meridian or YouthCare provider system
96 REJECTION Ordering/Prescribing/Referring
ISSUE: Ordering, prescribing, or referring provider type missing or incorrect
RESOLUTION:
- Step 1: Ensure the provider type on the claim is one the following: 010, 011, 012, 013, 016, 089 and is active in IMPACT
- Step 2: Verify for professional claims (CMS 1500) that the Provider TINs are in the appropriate fields. TINs are required on field 25, and the NPI should be inserted in the rendering provider field (field 24J) and the billing field (field 33).
- Step 3: Verify for facility/institutional claims (UB-04) that Provider TINs are listed in the appropriate fields. TINs are to be in field 5 and the facility NPI in field 56. Individual provider NPIs are required situationally in fields 76 - 79 (will vary per service performed).
- Step 4: Correct any issues with NPI and TIN locations on the claim and submit a first-time claim within 180 days from date of service
91 REJECTION: Invalid or Missing Taxonomy Code
ISSUE: Provider submitted incorrect, invalid, or missing taxonomy code
RESOLUTION:
Non-Waiver Providers
- Step 1: Review claim image to verify that the taxonomy code was billed in Box 24 and Box 33
- Step 2: Use the taxonomy code from claim image to confirm that the code is registered in IMPACT
- Step 3: Correct the missing or invalid taxonomy on the claim and resubmit claim as a first-time claim within 180 days from date of service
Waiver Providers
- Step 1: Review claim image to verify that the claim was billed with a Medicaid number in Box 33b as shown below. If submitting claims via the Meridian Secure Provider Portal, do not type in the G2 when entering the Medicaid number; the portal will automatically add it.
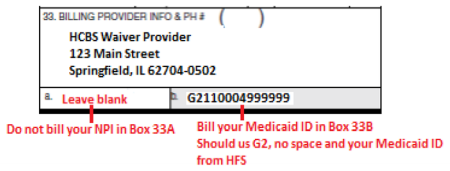
- Step 2: If the claim was billed with an NPI, remove and bill as a first-time claim with the IMPACT registered Medicaid number
- Step 3:If the claim was submitted with the correct Medicaid number and continues to reject 91, contact Provider Relations for assistance
REJECTIONS UB04 claims: Rejections Associated with Attending Physician
ISSUE: Provider submitted a UB04 claim with an invalid NPI for the attending physician in field 76. If the NPI is missing or invalid the following rejects may occur:
- 28 REJECTION: Attending Provider NPI Missing or Invalid
ISSUE: Provider submitted a claim with no attending provider NPI is received in field 76
RESOLTION: Correct the missing attending provider and resubmit claim as a first-time claim within 180 days from date of service - 03 REJECTION: Attending NPI Not Enrolled with State
ISSUE: Provider submitted a claim with an NPI in field 76, but the NPI is not IMPACT enrolled on the DOS
RESOLUTION:
- Step 1: If the claim was billed with an NPI not registered in IMPACT, update your IMPACT account by adding the missing NPI
- Step 2: Once the change is effective in IMPACT, resubmit the claim as a first-time claim within 180 days from date of service
- 45 REJECTION:Invalid or Missing Provider Type
ISSUE: Claim has an NPI that is in IMPACT and active on the DOS, but the NPI is not enrolled in IMPACT with a provider type of 010, 011, 012, 013, 016 or 089
RESOLUTION:
- Step 1: If the claim was billed with an NPI not registered in IMPACT with the appropriate provider type, update your IMPACT account by adding the missing provider type
- Step 2: Once the change is effective in IMPACT, resubmit claim as a first-time claim within 180 days from date of service
BW or BM REJECTION: Claim under review and Billed charges under review, no further action needed by the provider
ISSUE: Provider submitted a claim with a billed amount of $10,000,000 or more, or with more than 97 claim lines
RESOLUTION: No further action is required by the provider. The Meridian claim system cannot ingest claims with these parameters. Meridian has a process to monitor these rejects and manually key the claims into the Meridian system. Note that the finalized claims will have a different claim number assigned than the claim number received as a rejection.
Secure Provider Portals and Contact Information
Meridian Provider Services call 866-606-3700, Monday through Friday, from 8 a.m. to 5 p.m.
YouthCare Provider Services call 844-289-2264, Monday through Friday, from 8 a.m. to 5 p.m.
